Background
Hemophilia is a hereditary bleeding disorder, especially in severe hemophilia, that can lead to spontaneous bleeding. For hemophilia patients with inhibitors, even minor acute bleeding events or surgical procedures can have catastrophic consequences. Some hemophiliacs are forced to make surgical choices. There are many risks in perioperative period when hemophiliacs undergo major surgery. Seeking effective and safe perioperative clotting factor replacement therapy or bypass therapy is the basis of successful surgery.
Aims
To seek effective and safe perioperative coagulation factor replacement therapy or bypass therapy.
Methods
HA patients were treated with FVIII preparation during perioperative period. To calculate dosage, multiply the patient ' s weight in kilograms by the FVIII level in IU/dL desired, then multiply by 0.5. Example: 50 kg × 40 (IU/dL level desired) × 0.5 = 1000 IU of FVIII.
HB patients were treated with PCC or FIX during perioperative period. To calculate dosage, multiply the patient ' s weight in kilograms by the FIX level in IU/dL desired.
Example: 50 kg body weight × 40 (IU/dL level desired) = 2000 IU of plasma-derived FIX.
For hemophilia patients with low titer inhibitors, estimate the amount of FVIII required as a neutralizing inhibitor loading dose as recommended by WFH. The following formula is used to estimate the amount of FVIII needed as a loading dose to neutralize the inhibitor: [body weight (kg) × 80 × [(1 − hematocrit) × antibody titer (BU)]. An additional 50 IU/kg above the calculated loading dose is added to achieve a measurable FVIII activity.
Patients with hemophilia combined with high titer inhibitors were treated with rFVIIa combined with PCC SCBT regimen. Sequential use refers to alternating rFVIIa and aPCC every 3 hours.
Results
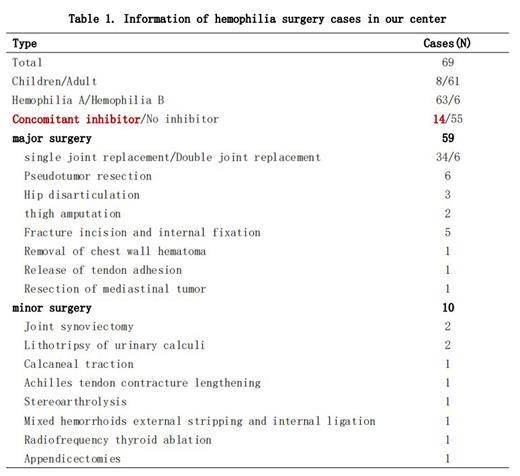
69 patients with indications for surgery and/or desire for surgery who underwent different types of surgery with clotting factor replacement therapy or bypass therapy were evaluated (Table 1). There were 37 cases of severe hemophilia and 32 cases of non-severe hemophilia. There were 63 cases of HA, including 50 cases of negative inhibitor and 13 cases of positive inhibitor. After meeting the inclusion and exclusion criteria, 69 patients were evaluated for different types of surgery under clotting factor replacement therapy or bypass therapy during perioperative period. 59 cases underwent major operations, including: 49 cases underwent joint replacement, among which 34 cases underwent single joint replacement and 6 cases underwent double joint replacement and so on. 10 cases underwent minor operations.
There were 14 cases of hemophilia with inhibitors, of which 13 were major operations with 175.38 (85.00-270.00) minutes of operation and 2 were minor operations with 45.00 minute of operation. In 12 patients with severe hemophilia and high titer inhibitors, the perioperative consumption of factor FVII was as follows: 447.62 (331.04-738.48)ug/kg on the day of surgery, and the total consumption was 2484.21 (1499.40-4500.00)ug/kg. The perioperative consumption of factor PCC was as follows: 126.10 (0-206.45)ug/kg on the day of surgery, and the total consumption was 1332.84 (529.20-1970.00)ug/kg.
The mean preoperative FVIII:C level of the HA patients was 1.19 (0.00~6.00)%, the mean preoperative FIX:C level was 0.022 (0.01~0.07)% of the HB patients.The average intraoperative blood loss of the 69 patients was 537.98 (0-3000) ml.
20 patients received intraoperative transfusion of blood products (red blood cells or fresh frozen plasma) and 49 patients did not receive intraoperative transfusion of blood products. In 55 hemophiliacs without inhibitor, no inhibitor was found after surgery.
Conclusion(s)
It is safe and effective to adopt different schemes for perioperative alternative therapy for different hemophilia types.
Disclosures
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal